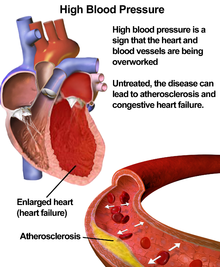
Hypertension (HTN or HT), also known as high blood pressure (HBP), is a long term medical condition in which the blood pressure in the arteries is persistently elevated.[1] High blood pressure usually does not cause symptoms. Long term high blood pressure, however, is a major risk factor for coronary artery disease, stroke, heart failure, peripheral vascular disease,vision loss, and chronic kidney disease.[3][4]
High blood pressure is classified as either primary (essential) high blood pressure or secondary high blood pressure.[5] About 90–95% of cases are primary, defined as high blood pressure due to nonspecific lifestyle and genetic factors.[5][6] Lifestyle factors that increase the risk include excess salt, excess body weight, smoking, and alcohol.[2][5] The remaining 5–10% of cases are categorized as secondary high blood pressure, defined as high blood pressure due to an identifiable cause, such aschronic kidney disease, narrowing of the kidney arteries, an endocrine disorder, or the use of birth control pills.[5]
Blood pressure is expressed by two measurements, the systolic and diastolic pressures, which are the maximum and minimum pressures, respectively.[2] Normal blood pressure at rest is within the range of 100–140 millimeters mercury (mmHg) systolic and 60–90 mmHg diastolic.[7] High blood pressure is present if the resting blood pressure is persistently at or above 140/90 mmHg for most adults.[5] Different numbers apply to children.[8] Ambulatory blood pressure monitoring over a 24-hour period appears more accurate than office best blood pressure measurement.[1][5]
Lifestyle changes and medications can lower blood pressure and decrease the risk of health complications.[9] Lifestyle changes include weight loss, decreased salt intake, physical exercise, and a healthy diet.[5] If lifestyle changes are not sufficient then blood pressure medications are used.[9] Up to three medications can control blood pressure in 90% of people.[5]The treatment of moderately high arterial blood pressure (defined as >160/100 mmHg) with medications is associated with an improved life expectancy.[10] The effect of treatment of blood pressure between 140/90 mmHg and 160/100 mmHg is less clear, with some reviews finding benefit[11][12] and others finding a lack of evidence for benefit.[13] High blood pressure affects between 16 and 37% of the population globally.[5] In 2010 hypertension was believed to have been a factor in 18% (9.4 million) deaths.[14]
Signs and symptoms[edit]
Hypertension is rarely accompanied by symptoms, and its identification is usually through screening, or when seeking healthcare for an unrelated problem. Some with high blood pressure report headaches (particularly at the back of the head and in the morning), as well as lightheadedness, vertigo, tinnitus (buzzing or hissing in the ears), altered vision orfainting episodes.[15] These symptoms, however, might be related to associated anxiety rather than the high blood pressure itself.[16]
On physical examination, hypertension may be associated with the presence of changes in the optic fundus seen by ophthalmoscopy.[17] The severity of the changes typical ofhypertensive retinopathy is graded from I–IV; grades I and II may be difficult to differentiate.[17] The severity of the retinopathy correlates roughly with the duration and/or the severity of the hypertension.
Hypertensive crisis
Severely elevated blood pressure (equal to or greater than a systolic 180 or diastolic of 110) is referred to as a hypertensive crisis. Hypertensive crisis is categorized as eitherhypertensive urgency or hypertensive emergency, according to the absence or presence of end organ damage, respectively.[19][20]
In hypertensive urgency, there is no evidence of end organ damage resulting from the elevated blood pressure. In these cases, oral medications are used to lower the BP gradually over 24 to 48 hours.[21]
In hypertensive emergency, there is evidence of direct damage to one or more organs.[22][23] The most affected organs include the brain, kidney, heart and lungs, producing symptoms which may include confusion, drowsiness, chest pain and breathlessness.[21] In hypertensive emergency, the blood pressure must be reduced more rapidly to stop ongoing organ damage,[21] however, there is a lack of randomised controlled trial evidence for this approach.[23]
Children[edit]
Failure to thrive, seizures, irritability, lack of energy, and difficulty in breathing[27] can be associated with hypertension in neonates and young infants. In older infants and children, hypertension can cause headache, unexplained irritability, fatigue, failure to thrive, blurred vision, nosebleeds, and facial paralysis.[27][28]
Causes[edit]
Primary hypertension[edit]
Main article: Essential hypertension
Hypertension results from a complex interaction of genes and environmental factors. Numerous common genetic variants with small effects on blood pressure have been identified[29] as well as some rare genetic variants with large effects on blood pressure.[30] Also, GWAS have identified 35 genetic loci related to blood pressure; 12 of these genetic loci influencing blood pressure were newly found.[31] Sentinel SNP for each new genetic loci identified has shown an association with DNA methylation at multiple nearbyCpg sites. These sentinel SNP are located within genes related to vascular smooth muscle and renal function. DNA methylation might affect in some way linking common genetic variation to multiple phenotypes even though mechanisms underlying these associations are not understood. Single variant test performed in this study for the 35 sentinel SNP (known and new) showed that genetic variants singly or in aggregate contribute to risk of clinical phenotypes related to high blood pressure.[31]
Blood pressure rises with aging and the risk of becoming hypertensive in later life is considerable.[32] Several environmental factors influence blood pressure. High salt intake raises the blood pressure in salt sensitive individuals; lack of exercise, obesity, and depression[33] can play a role in individual cases. The possible role of other factors such as caffeine consumption,[34] and vitamin D deficiency[35] are less clear. Insulin resistance, which is common in obesity and is a component of syndrome X (or the metabolic syndrome), is also thought to contribute to hypertension.[36] Events in early life, such as low birth weight, maternal smoking, and lack of breast feeding may be risk factors for adult essential hypertension, although the mechanisms linking these exposures to adult hypertension remain unclear.[37] An increased rate of high blood urea has been found in untreated people with hypertensive in comparison with people with normal blood pressure, although it is uncertain whether the former plays a causal role or is subsidiary to poor kidney function.[38]
Secondary hypertension[edit]
Main article: Secondary hypertension
Secondary hypertension results from an identifiable cause. Kidney disease is the most common secondary cause of hypertension.[18] Hypertension can also be caused by endocrine conditions, such as Cushing's syndrome, hyperthyroidism, hypothyroidism, acromegaly, Conn's syndrome or hyperaldosteronism, hyperparathyroidism andpheochromocytoma.[18][39] Other causes of secondary hypertension include obesity, sleep apnea, pregnancy, coarctation of the aorta, excessive eating of liquorice, excessive drinking of alcohol, and certain prescription medicines, herbal remedies and illegal drugs.[18][40] Arsenic exposure through drinking water has been shown to correlate with elevated blood pressure.[41][42]
Pathophysiology[edit]
Main article: Pathophysiology of hypertension
In most people with established essential hypertension, increased resistance to blood flow (total peripheral resistance) accounts for the high pressure while cardiac output remains normal.[43] There is evidence that some younger people with prehypertension or 'borderline hypertension' have high cardiac output, an elevated heart rate and normal peripheral resistance, termed hyperkinetic borderline hypertension.[44] These individuals develop the typical features of established essential hypertension in later life as their cardiac output falls and peripheral resistance rises with age.[44] Whether this pattern is typical of all people who ultimately develop hypertension is disputed.[45] The increased peripheral resistance in established hypertension is mainly attributable to structural narrowing of small arteries and arterioles,[46] although a reduction in the number or density of capillaries may also contribute.[47] Whether increased active arteriolarvasoconstriction plays a role in established essential hypertension is unclear.[48] Hypertension is also associated with decreased peripheralvenous compliance[49] which may increase venous return, increase cardiac preload and, ultimately, cause diastolic dysfunction.
Pulse pressure (the difference between systolic and diastolic blood pressure) is frequently increased in older people with hypertension. This can mean that systolic pressure is abnormally high, but diastolic pressure may be normal or low a condition termed isolated systolic hypertension.[50] The high pulse pressure in elderly people with hypertension or isolated systolic hypertension is explained by increasedarterial stiffness, which typically accompanies aging and may be exacerbated by high blood pressure.[51]\
Many mechanisms have been proposed to account for the rise in peripheral resistance in hypertension. Most evidence implicates either disturbances in the kidneys' salt and water handling (particularly abnormalities in the intrarenal renin-angiotensin system) and/or abnormalities of the sympathetic nervous system. These mechanisms are not mutually exclusive and it is likely that both contribute to some extent in most cases of essential hypertension. It has also been suggested that endothelial dysfunction and vascular inflammationmay also contribute to increased peripheral resistance and vascular damage in hypertension. Interleukin 17 has garnered interest for its role in increasing the production of several other immune system chemical signals thought to be involved in hypertension such as tumor necrosis factor alpha, interleukin 1, interleukin 6, and interleukin 8.